Diastasis Recti and Postnatal Recovery tips for the First 6 Weeks and Beyond
Pregnancy and birth challenge the body in incredible ways. One condition that affects at least 60% of women during and after pregnancy is called abdominal wall separation, or diastasis recti.
For over a decade, I have been working closely with women to help them navigate the physical challenges of this journey into motherhood - preparing women to birth with strength and confidence, guiding them as they recover postnatally, and coaching mothers and grandmothers as they reclaim core health years or even decades later. This condition is one that I have often helped women heal from.
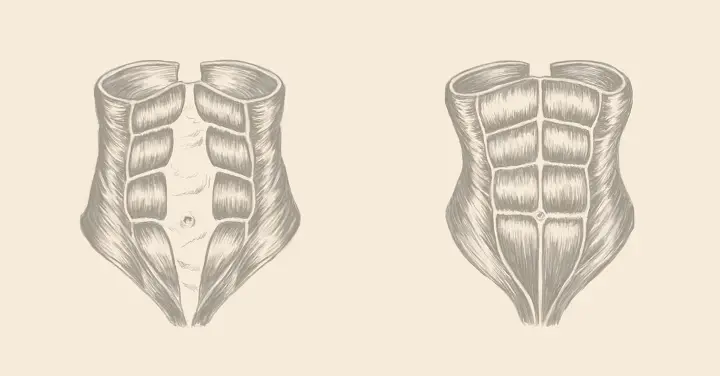
Diastasis recti occurs when the rectus abdominis (your 6-pack muscles) separate due to the pressure placed on the linea alba during gestation. Abdominal wall separation is a thinning and weakening of the connective tissue caused by your growing fetus. It is not a tear (that’s either a ventral hernia or an umbilical hernia). Diastisis recti can linger years after pregnancy and is the primary reason women show sooner in their second and subsequent pregnancies.
Diastasis recti has often been dismissed by medical providers as a cosmetic concern, but the condition carries very real health implications. When the abdominal muscles separate, core function suffers leaving many women with heightened symptoms of lower back pain, urinary leaking, pelvic floor dysfunction, and prolapse. Thankfully, there are postnatal exercises to fix diastasis recti.
The first six weeks: restorative movement
Movement during the earliest weeks after birth should be gentle, nourishing, and replenishing. Here are three restorative physical practices I recommend incorporating into your daily routine as soon as you feel ready postpartum, all of which support health and function while paving the way for a safe return to more vigorous activity when you’re cleared by your doctor or midwife.
1. Reconnect with your core, breath and pelvic floor.
While seated upright or lying on your back with your spine lengthened and knees bent, take a few full, expansive breaths. With each inhalation, allow your belly and pelvic floor to soften and relax, filling your torso with air. Then exhale with strength as you engage your abdominal muscles and your pelvic floor in an upward lift toward the spine. Repeat this 2-3 times.
After a few full, diaphragmatic breaths, transition to Core Compressions:
- Step 1: Release and relax your abs and pelvic floor as you take a shallow breath.
- Step 2: Exhale as you gently Kegel* and squeeze your abdominal muscles in a subtle, upward rolling lift toward the spine. *Note: If you suffer from chronic constipation, pelvic pain, or pain during intercourse, skip the Kegel in this exercise. Instead, maintain a relaxed pelvic floor and contact a pelvic health physical therapist.
- Repeat the above steps for 1-2 minutes. Each repetition should be slow and controlled. Pause as needed to take a full, diaphragmatic breath.
Do one set per day for a few days, and gradually add another until you reach a total of 10 minutes per day - (spread out or performed all at once). These Core Compressions should feel like light to moderate work. Listen to your body, and stop if anything feels painful or simply “not right.”
2. Walk with a friend/partner (preferably outside).
Begin with as little as 5 minutes of walking and talking, with the baby in a stroller or in a carrier worn by your partner. Weather permitting, walk outside when you feel up to it. Gradually lengthen the duration of your walk from 5 minutes to 10, 15 and eventually 30 minutes. Let this be a social time and a welcomed break from attending to the needs of your newborn. As you feel stronger and more independent, go for a solo walk in nature if that feeds your soul. You have just entered an entirely new chapter of life; be gracious with yourself and with your body.
Both of the above practices will prepare you for more physically strenuous activities when your doctor or midwife clears you for that, typically 4-6 weeks after a vaginal delivery and 6-8 weeks following a C-section.
3. Strive for healthy, neutral posture and alignment.
Given the exhaustion of new motherhood, it’s easy to forget good posture habits. But healthy posture is more important during the early postpartum period than ever and tiny adjustments can yield big results. Several times a day, perform a quick posture self-check.
- Bring your attention to your body and your breath.
- Take a full, diaphragmatic breath.
- As you exhale, think about rolling your shoulders back and lengthening your spine while keeping your ribs anchored, and your pelvis neutral - neither spilling forward nor tucking under.
Whether seated, standing, walking or pushing a stroller, healthy posture facilitates core recovery and healthy circulation, while boosting strength and stamina for daily life.
Beyond the first six weeks: when you are cleared for full activity, avoid these common mistakes
It’s important to remember that even after your doctor or midwife gives you the green light to resume full activity, that you are still at risk of making your abdominal wall separation worse. While not all of the pre-baby exercises you loved are damaging, there are a number of exercises to avoid with diastasis recti.
1. Skip or modify any exercise or activity that bulges your abdomen forward.
This is by no means a complete list, but here are some of the worst offenders. Avoid:
- Sit-ups
- Pilates “hundreds”
- Crunches (all varieties)
- Supine (laying down on your back) double leg lifts
- Boat pose
The primary question to ask yourself while performing any exercise is, “can I do this without bulging my abs forward?” If not, modify it (perform a single leg lift instead of lifting both legs, for instance) or skip it entirely.
2. Wait to resume high impact activities.
It’s important to wait to reintroduce running, jogging, jumping, or trampoline workouts into your routine until you are at least 12 weeks postpartum and can perform a light jog or several jumping jacks without:
- Leaking urine
- Feeling bladder pressure or urgency to pee
- Experiencing downward pressure on your pelvic floor
If you detect any of these symptoms, you are not ready for high impact activities. Continue to focus on core and pelvic core strengthening, and then try again in a few weeks. If symptoms persist, see a pelvic floor physical therapist for an evaluation.
3. Avoid splaying the ribs.
When you stretch to the point that your lower ribs splay outward, your upper abdominal muscles, which insert into the lower ribs, also separate. Modify or keep your range of motion moderate when performing chest-openers in yoga, such as upward dog or cobra. Replace full wheel with a bridge pose, and be mindful of keeping your ribs anchored.
There’s no reason to live with the symptoms of abdominal wall separation; from low back pain, to pelvic dysfunction, incontinence and prolapse these complications are not your new normal. The key to healing - from the early postpartum period and beyond - starts with restorative movement and continues with therapeutic exercise that protects your core strength, integrity, and function. To learn more about the best and worst diastasis recti exercises and how to modify your favorite workouts using core-safe principles visit every-mother.com.

Leah Keller is a certified personal trainer and the founder of Every Mother, an online exercise program endorsed by medical and birth professionals worldwide. With over two decades of fitness experience, Leah empowers and equips women to prepare for labor and restore core strength and function postnatally – no matter how long it’s been. Leah has been featured as a women’s health expert by major media outlets, including NPR, goop and Good Morning America.